2022년 5월 2일에 아르헨티나의 Hospital Privado de Rosario의 AMI 코드 코디네이터이자 중재 심장전문의인 Ignacio Cigalini 박사가 63세 남성을 대상으로 카테터경유 대동맥 판막 치환술(TAVR)을 실시합니다.
이전 수술 위에 교체 밸브를 고정하기 위해 카테터를 사용하는 TAVR 시술은 기존 수술에 비해 몇 가지 이점이 있지만 급성 뇌졸중의 위험이 높습니다. 모든 예방조치에도 불구하고, 환자는 뇌졸중을 겪습니다.
오후 1시 12분에 Hospital Privado de Rosario의 스피커가 Code Stroke를 발표합니다.
치료 기간은 기록적인 10분이며, 이 기간 동안 병원 신경학과장인 Dr Guadalupe Maria Bruera가 여러 가지 삶을 변화시키는 결정을 내릴 것입니다.
병원 내 뇌졸중 대 지역사회 발병 뇌졸중
2015년 신경병원 전문의에게 발표된 University of Colorado School of Medicine의 Dr Ethan Cumbler가 발표한 병원 내 허혈성 뇌졸중에 대한 논문에 따르면, 다른 진단 또는 시술을 위해 입원한 환자에서 급성 치료 입원 중에 모든 뇌졸중의 최대 17%가 발생합니다. 이 중 절반에서 2/3는 수술 전후 및 시술 전후이며, 심장 수술 환자는 위험이 가장 큽니다.
병원 내 뇌졸중은 지역사회 발병 뇌졸중보다 결과가 상당히 나쁘며, 이는 고령이고 이미 아프며 혈전용해술에 대한 내과적 또는 외과적 금기증이 높은 환자에서 발생하기 때문일 뿐만 아니라, 병원 내 뇌졸중은 또한 평가와 치료가 더 오래 지연되는 경향이 있습니다.
2022년 2월 미국심장협회의 과학적 진술은 병원 내 뇌졸중 환자가 응급실 환경에서 뇌졸중 환자에 비해 증상 인식부터 신경영상검사까지 유의하게 긴 간격을 가진다는 증거를 인용 뇌졸중 한다(4.5시간 대 1.2시간). Get With The Guidelines 레지스트리의 한 연구에서는 지역사회 발병 뇌졸중에 비해 뇌졸중 인식에서 혈전용해술까지 경과한 시간이 60분에 비해 81분으로 더 길었다는 것을 발견했습니다.
이러한 이유에는 환자가 입원한 질병, 진정 또는 마취 효과 또는 약물의 부작용에 잘못 기인한 뇌졸중 증상이 포함됩니다. 지역사회 발병 뇌졸중 환자와 달리, 병원 내 뇌졸중의 피해자는 긴급한 문화로 응급실을 통해 시스템에 들어가지 않습니다. 오히려, 뇌졸중 진단 경험이 없고 빠른 행동의 중요성에 대한 인식이 낮은 직원이 이들을 돌볼 가능성이 높습니다.
소중한 10분
로사리오의 63세 시민은 운이 좋은 사람 중 하나입니다. Dr. Cigalini는 Hospital Privado de Rosario의 다른 모든 사람들과 마찬가지로 매달 실시되는 뇌졸중 코드 교육에 정기적으로 참석하며 뇌졸중 발생 시 즉각적인 조치의 중요성을 잘 알고 있습니다 뇌졸중. 환자가 실어증을 보인다는 것을 알게 되면 잠시 주저하지 않고 Code Stroke를 활성화합니다.
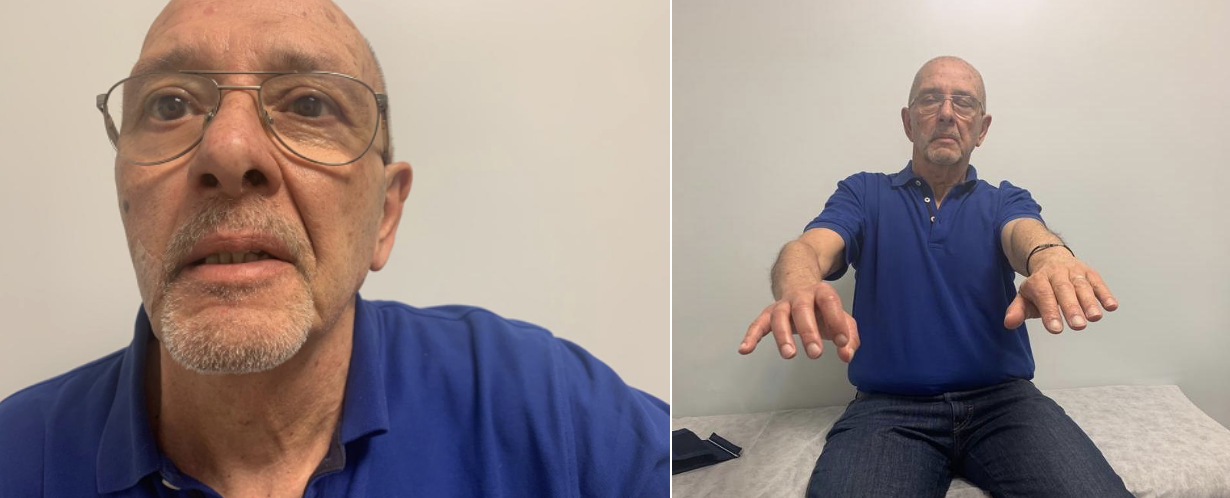
카테터 삽입기실에서 촬영실까지 가까운 거리로 이송되는 동안, 신경과 전문의 Dr Guadalupe Bruera의 NIHSS 평가는 12점을 제공합니다. 자기 공명 혈관 조영술을 사용하면 출혈을 배제하고 M3에서 왼쪽 중간 대뇌 동맥으로의 분절 폐색 위치를 찾는 데 2분밖에 걸리지 않습니다. Bruera 박사는 외과적 혈전제거술로 혈전에 도달할 수 없음을 인지하고 혈전용해술을 결정합니다. 그녀는 볼루스를 직접 투여합니다. 나머지 주입은 환자가 60분 동안 머무르는 ICU에서 실시합니다.
Cigalini 박사는 치료 결정에 정보를 제공하는 중요한 데이터를 제공하고 환자 가족과의 의사소통을 관리하는 등 전체 과정에 계속 참여해 왔습니다.
뇌졸중 코드 활성화부터 치료까지 전체 프로세스에 10분의 귀중한 시간이 소요되었습니다.
모든 사람의 업무를 존중해야 합니다.
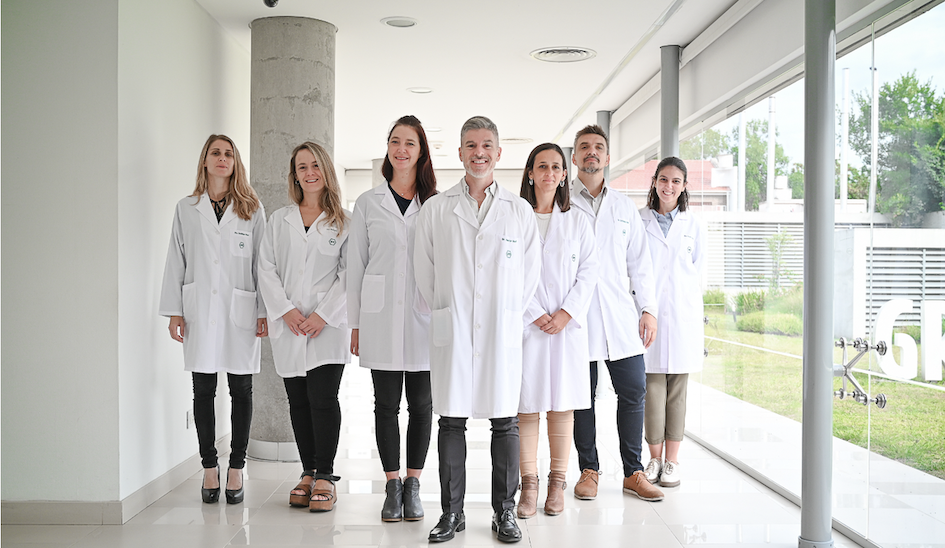
Hospital Privado de Rosario는 매년 약 219명의 뇌졸중 환자를 인정하며, 지역사회 발병 뇌졸중에 대한 평균 DTN 시간은 40분입니다. 병원 내 뇌졸중에 대한 평균 치료 시간은 35분으로 추세를 뒤흔듭니다. Bruera 박사는 명확한 구조화된 뇌졸중 코드 프로토콜과 다학제적 팀워크에 대한 설명이라고 말합니다. 병원 내 뇌졸중의 최적의 관리를 위해 정기적인 뇌졸중 코드 교육에는 병원 전체의 모든 부서의 직원이 참여합니다. 그 결과, 뇌졸중이 의심될 때 신속하게 행동해야 할 필요성에 대한 인식이 넓어지며, 모든 사람은 Code Stroke가 발표될 때 훈련을 알고 있습니다.
고도로 조직화된 환자 경로는 치료 지연을 최소화하고, Angels 이니셔티브가 진행하는 시뮬레이션은 개선 기회를 찾는 데 도움이 되지만, 팀워크는 결정적인 요소이며, 계층이 편평해지면 팀의 모든 사람을 동원하는 데 도움이 됩니다.
Bruera 박사는 “뇌졸중의 기본 측면 중 하나는 과시입니다.”라고 말합니다. “10~15명의 의료 전문가가 간호 및 행정 직원과 함께 뇌졸중 코드에 참여합니다.
"이 팀의 모든 구성원은 반드시 권한을 부여받았다고 느껴야 합니다. 교육뿐만 아니라 예시를 통해 얻을 수 있는 것입니다. 뇌졸중 코드를 조정하는 한 사람이 있지만, 모든 사람의 업무를 존중해야 합니다.
"성공적인 뇌졸중팀 지식 구축이 항상 집단적이라는 원칙을 기반으로 합니다. 개인적으로 배울 수 있는 것은 없습니다.”

인간의 기본적인 선의
Rosario의 10분 "기적"은 부분적으로만 조직과 교육의 결과라는 것이 분명합니다. 이 뇌졸중팀 성공은 원칙에도 뿌리를 두고 있으며, HPR에서 뇌졸중 관리를 관장하는 원칙은 Dr Bruera의 개인적 가치와 분리할 수 없습니다.
그녀는 자신을 "매일 배우고자 하는 사람"으로, 자신의 병원을 "환자, 간호사, 비서 및 동료로부터 많은 것을 배웁니다"라고 설명합니다.
그녀의 병원과 특히 심장학 분야의 동료들이 진료한 의약품의 질은 그녀가 다른 곳에서 경력을 쌓을 기회를 얻기 위해 Rosario를 선택한 이유 중 하나입니다.
그녀는 "저는 모든 결점, 특히 로사리오시에서도 우리나라를 깊이 사랑합니다."라고 말합니다.
땅에 대한 사랑과 학습은 가족의 유산입니다. Bruera 박사와 그녀의 형제는 심리학자 어머니와 신경과 의사 아버지가 자랐으며, 둘 다 선생님이기도 합니다. 그녀는 "저는 다른 사람을 지지하고 존중하는 등 인간의 기본적인 선의를 반영하는 핵심 가치를 가진 가족에서 자랐습니다."라고 말합니다.
이러한 가치는 Hospital Privado de Rosario의 뇌졸중 프로그램에서 표현되며, 조직된 경로 및 분할된 두 번째 의사 결정과 함께 때때로 10분 내에 기적을 전달할 수 있습니다.




