
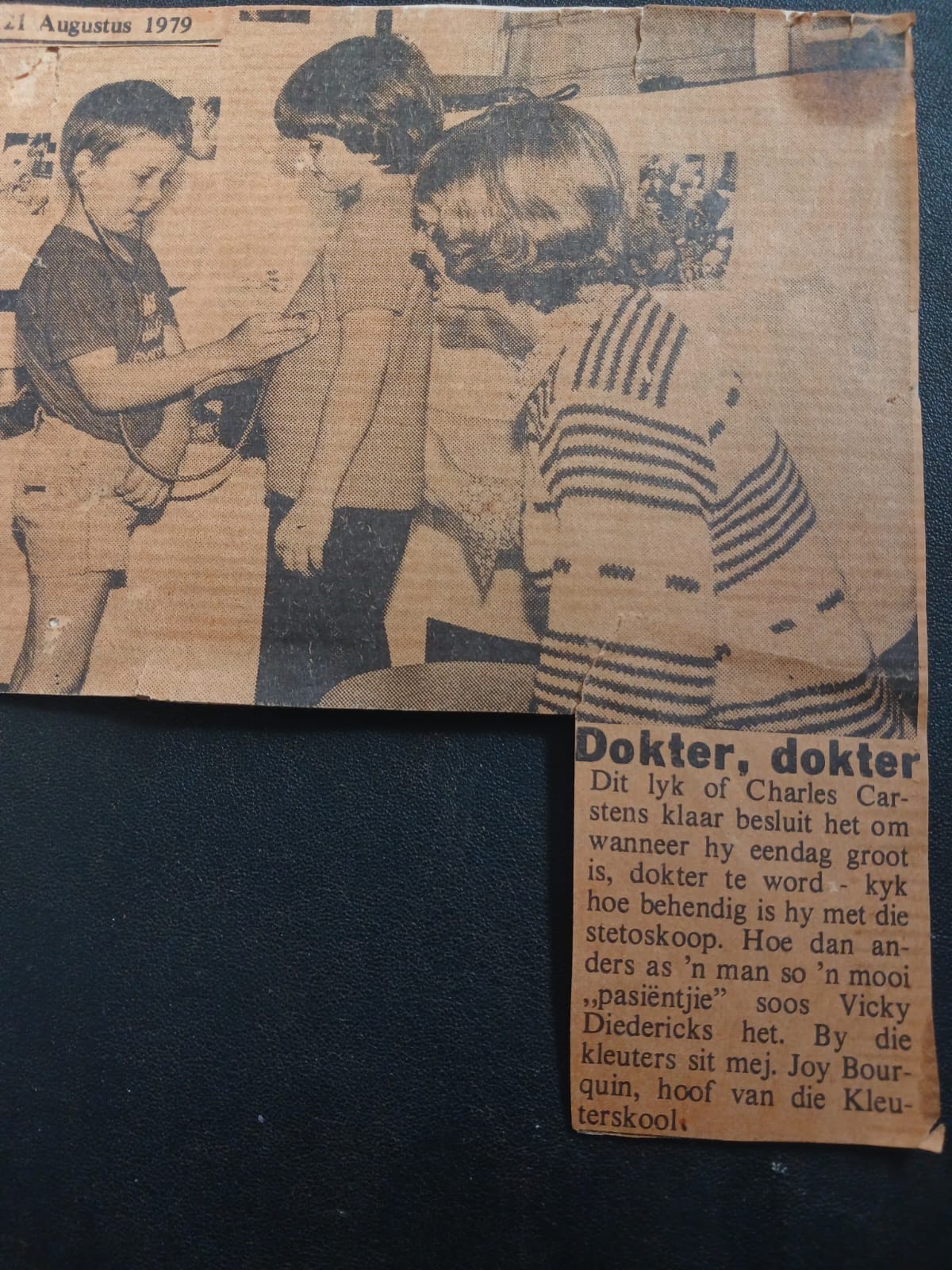
1979년 8월, 4세의 한 지역 신문에 동료 유치원의 마음을 듣는 척하는 사진이 나왔습니다. 첨부된 문구에서, 그 소년은 “의사” Charl Carstens로 식별되었습니다. 의지 또는 운명? 귀하는 결정을 내리셨습니다. Charl Carstens 박사는 이제 7가지 자연 경이로움 중 하나를 보여주는 사진 엽서를 가지고 대형 민간 병원의 응급실을 이끌고 있기 때문입니다.
Netcare Blaauwberg Hospital은 테이블 마운틴의 고전적인 전망으로 유명한 케이프 타운의 해변 교외인 Bloubergstrand에 위치해 있습니다. 2007년에 문을 연 이 병원은 즉시 역사를 쌓았습니다. 그 이유는 응급실이 남아프리카에서 응급의약품 전문가들에 의해 최초로 설립되었기 때문입니다.
Clive Balfour 박사는 2003년에 남아프리카에서 전문 분야로서 응급 의약품을 도입했습니다. Charl은 영국 레이크 디스트릭트의 한 병원에서 교대 근무하면서 Balfour 박사를 우연히 만났으며, 남아프리카 공화국으로 복귀하여 4년간의 코스를 이수한 10명의 남아프리카 의사로 구성된 첫 번째 그룹 중 하나가 되는 것을 장려받았습니다. 한 동료 레지던트가 2007년 파트타임으로 근무한 후 Netcare Blaauwberg와 Charl에 응급실을 설립했으며, 2008년에 컨설턴트로 풀타임으로 합류했습니다.
그는 2018년에 남아프리카 외상 학회(TSSA)로부터 III급 외상 센터로 인정을 받은 후, 2023년에 II급 외상 센터 인증을 받기 위해 모든 정류장을 꺼냈습니다.
Angels 이니셔티브의 전구물질이 2014년 남아프리카에서 사업을 시작했을 때, Netcare Blaauwberg는 뇌졸중 치료 상태를 획득한 최초의 병원 중 하나였습니다. 2018년에 Angels 컨설턴트가 병원에서 시뮬레이션을 실시했고, Angels 뇌졸중 키트와 체크리스트가 뇌졸중 프로토콜의 일부가 되었습니다. 그러나 뇌졸중 프로그램에 대한 열정은 Covid가 의료 시스템을 붕괴시키고 병원이 신경과 전문의와 뇌졸중 챔피언을 질병으로 잃은 후 표식되었습니다. 하지만 그 모든 것이 곧 변할 것입니다.

Sr Claudette Lotz는 간호 이외의 어떤 분야에서도 경력을 고려한 적이 없습니다. “아시다시피, 너도 알겠지.”라고 그녀는 말합니다. 그녀는 현재 요하네스버그 대학에서 1학위를 받았으며, 1년 후 ICU에서 외상 간호사로 Netcare 그룹에 합류했습니다. 일상 생활을 싫어하면서 응급실에 입원했습니다. “병동에서 일한 적이 없습니다”라고 그녀는 말합니다.
그녀의 아이들이 주 수영가가 되었을 때, 그녀의 커리어는 뒤에서 앉았습니다. 거의 20년 동안 그녀는 가끔씩만 근무했지만, 2019년에는 케이프 타운으로 이사하여 풀타임 간호로 복귀할 준비를 했습니다. 같은 해에 그녀는 University of Stellenbosch에서 간호 교육에 대한 대학원 자격을 취득했습니다. 다음 해에는 팬데믹 기간 동안 공중 보건에 대한 대학원 과정을 시작했으며, 지난 12월에는 간호 과학 석사 학위를 취득했습니다. 2022년 9월, 그녀는 Netcare Blaauwberg의 ED 부서 단위 관리자가 되었으며, 1년이 지나지 않아 병원이 첫 번째 금색 WSO Angels 어워드를 수상했습니다.
그녀는 뇌졸중 치료 시스템이 이미 마련되어 있고, Carstens 박사가 즉시 합류했다고 말합니다. 품질 모니터링이 개선의 핵심임을 인식한 Claudette는 Netcare 그룹의 국가 뇌졸중 코디네이터인 Sr Zasskia Wiese를 만나 뇌졸중 치료 품질 개선 레지스트리인 RES-Q에 환자 데이터를 로드하는 방법을 배웠습니다.
“처음에는 불가능해 보였어요”라고 그녀는 말합니다. “그러나 일단 시작하면 할 수 있다는 것을 알 수 있습니다.” 그녀는 ED 임상 간호사 전문가인 Michelle Cronje와 함께 매일 아침 뇌졸중 치료 데이터를 로드하는 것을 최우선으로 하기 시작했습니다. 그 수치에서 DTN 시간이 더 빨라질 수 있는 것으로 나타났을 때, Angels 컨설턴트인 Bernise Schubert는 hyperacute 단계에 대한 교육을 촉진했습니다. 방사선과에 도달하기까지의 시간이 어려움을 제기했을 때, 그들은 EMS에 뇌졸중 환자를 CT로 직접 데려와 실행 시 검사를 실시하도록 요청했습니다. 주요 플레이어를 연결하는 Whatsapp 그룹은 엄청난 가치를 입증했으며 사전 알림 지원하여 앰뷸런스를 호출하는 순간부터 CT에 도착할 때까지 환자를 인식합니다.
이러한 노력의 결과는 2023년 3분기에 두 번째 금상을 수상한 후 4분기에 첫 번째 백금상을 수상한 것입니다. 이제 그들은 두 번째 다이아몬드 상을 수상하게 되며, 이를 우수한 뇌졸중 케어의 경주로 인정하게 됩니다.

Charl은 응급실 의사들 사이에 태도의 변화가 있었다고 말합니다. 이들은 혈전용해술로 허혈성 뇌졸중을 치료할 이유를 적극적으로 찾고, 이 삶을 변화시키는 치료에 대한 가족의 동의를 얻기 위해 모든 노력을 기울입니다. 젊은 세대의 간호사들의 열정과 그들이 치료의 영향을 목격할 때 그들의 흥분도 마찬가지로 전염성이 있습니다.
“데이터 로딩을 시작하면 첫 번째 기본 단계를 시작하면 됩니다”는 Claudette가 아직 뇌졸중 치료 개선을 약속하지 않은 병원에 대해 어떤 조언을 해 주었는지 물어볼 때의 답변입니다.
Charl은 "첫 걸음을 내디뎌내는 것은 어려울 수 있습니다."라고 덧붙입니다. "그러나 불을 밝힐 준비가 된 사람이 필요합니다. 그러면 모든 것이 제자리에 놓입니다.”
두 사람 모두 서로 다른 방식으로도 마찬가지입니다. Charl은 응급 의사에게 필요한 특성이라고 말하는 멋진 머리를 가지고 있습니다. “ED는 카우보이를 위한 장소가 아닙니다. 혼란스러운 스트레스 상황을 관리하고 좋은 결과 얻기 위한 질서를 만들기 위해 멋진 머리가 필요합니다.” 그는 직장과 가족 생활을 망치고 여전히 골프 경기를 치려고 하는 어린 아버지입니다.
다른 인생의 단계에서 그녀가 좋아하는 분야에서 자신의 경력을 재탄생시킨 Claudette는 직장에서 벗어나기 어렵다고 생각합니다. 그녀는 밤에 10시 또는 11시가 될 때까지 일할 가능성이 높으며, 특히 부서가 바쁘고 팀이 손을 꽉 찬 경우 그러합니다. “저는 서서 다른 사람이 고생하는 것을 볼 수 없습니다. “리더는 팀의 일원이어야 합니다.”
Charl과 Claudette는 성공하기 위해 노력하고 있으며, 병원에 대해 큰 자부심을 느끼고 있습니다. 이제 Charl과 Claudette는 다이아몬드를 더욱 밝게 빛낼 수 있는 방법을 모색하고 있습니다. 이들은 뇌졸중 발병 시간이 알려지지 않은 환자가 혈전용해술의 후보자인지 판단하기 위해 MRI 기법인 DWI-FLAIR 불일치를 사용하는 것에 대해 방사선과 팀과 이야기하고 있습니다.
각성 뇌졸중과 늦게 도착하는 환자를 위한 뇌졸중 프로토콜은 더 많은 생명을 구할 것입니다. 심지어 중증 뇌졸중을 겪은 후 너무 늦게 도착한 찰의 삼촌의 생명을 구했을 수도 있습니다. 그때까지는 아무것도 할 수 없었다고 Charl은 말합니다. “아마도 지금 할 수 있었을 것 같습니다.”



