고기능 폴란드 병원의 경로 시뮬레이션은 이웃 병원뿐만 아니라 새로운 의사들에게도 학습의 기회였으며, 선의의 의무가 더 나아질 것임을 상기시켜 주었습니다.

폴란드 북부에 있는 올슈틴의 지역 병원이 어떻게 약 10분의 도착 후 치료 시간을 달성하는지 알고 싶다면, 문 밖에서 답을 찾을 수 있습니다. 병원 입구에서 앰뷸런스가 올라가 뇌졸중 환자가 이송 중임을 알렸을 때, 입구 안에 신경과 전문의가 대기하고 있습니까? 아니요, 그렇지 않습니다.
그 이유는 통화 중인 젊은 뇌졸중 의사가 이미 앰뷸런스 안에서 뛰어들어 환자를 구하기 위해 1초가 아니라는 결정을 내렸기 때문입니다.
이 의사에게는 그 순간 그 어떤 것도 중요한 것이 아니라고 Angels 컨설턴트인 Agnieszka Tymecka-Woszczerowicz는 말합니다. 그는 4년 후에도 여전히 현장에서 헌신을 온전히 표현하고 있습니다. “그는 모든 환자를 가족처럼 대합니다.”
모든 뇌졸중 환자에게 가능한 최상의 치료를 제공하고자 하는 열망은 올즈틴의 종합 센터이자 와르미아 및 마주리 지역의 선도적인 의료 기관인 Voivodeship Specialist Hospital의 인상적인 치료 시간으로 이어졌으며, 몇 년 전 올즈틴에서 여러 목표를 세웠던 즉흥적인 경로 시뮬레이션의 동기였습니다.
도어 열기
올츠틴의 Voivodeship Specialist Hospital은 기계적 혈전제거술로 뇌졸중 환자를 치료할 수 있는 능력을 갖춘 폴란드의 20개 병원 중 하나입니다. 3,800만 명 이상의 인구에 서비스를 제공하기 위해 38개의 종합 센터가 필요한 것으로 추정되지만, 이 수치는
은 2019년에 약 300명의 신경과 전문의들로 구성된 회의를 발표한 뛰어난 정신상 수상자 안나 크즈워곤코우스카 교수의 리더십을 증명합니다. “엔Angels 문을 두드리면 열어야 한다는 점을 기억하십시오.”
그 후 4년 동안 폴란드의 Angels 팀은 이 나라의 변화하는 요구에 맞게 프로그램을 조정했으며, 여기에는 혈전제거술 경로 관리를 위한 지역 교육 촉진, 대혈관 폐색을 진단하기 위한 CT 혈관조영술 스캔 해석에 관한 워크숍과 웨비나 등이 포함되었습니다.
혈전용해술 치료 시간을 단축하기 위한 주요 도구인 시뮬레이션 교육은 일반적으로 DTN 경로에 중점을 둡니다. 기계적 혈전제거술에 더 많은 노력을 기울이는 경로 시뮬레이션은 교육 의제에서 덜 자주 이루어지지만, 올츠틴 Voivodeship Specialist Hospital의 팀은 시계를 기준으로 DTN 성능을 테스트할 뿐만 아니라 서혜부까지 이어지는 경로의 장벽을 식별하기로 결정되었습니다.

순간 포착
Voivodeship Specialist Hospital은 이 지역을 여행하면서 올스젠 주변의 여러 주요 뇌졸중 센터에서 시뮬레이션 교육을 실시하면서 아그니에스차 목록에 등재되지 않았습니다. 그러나 그녀는 이 선도적인 병원의 뇌졸중 병동 책임자가 된 후 입원 기간을 연장해야 했으며, 보다 숙련된 팀이 마찬가지로 자신의 성과를 검토함으로써 혜택을 볼 수 있다고 선언했습니다.
Agnieszka는 "잠시 시간을 잡는 것"을 회상합니다.
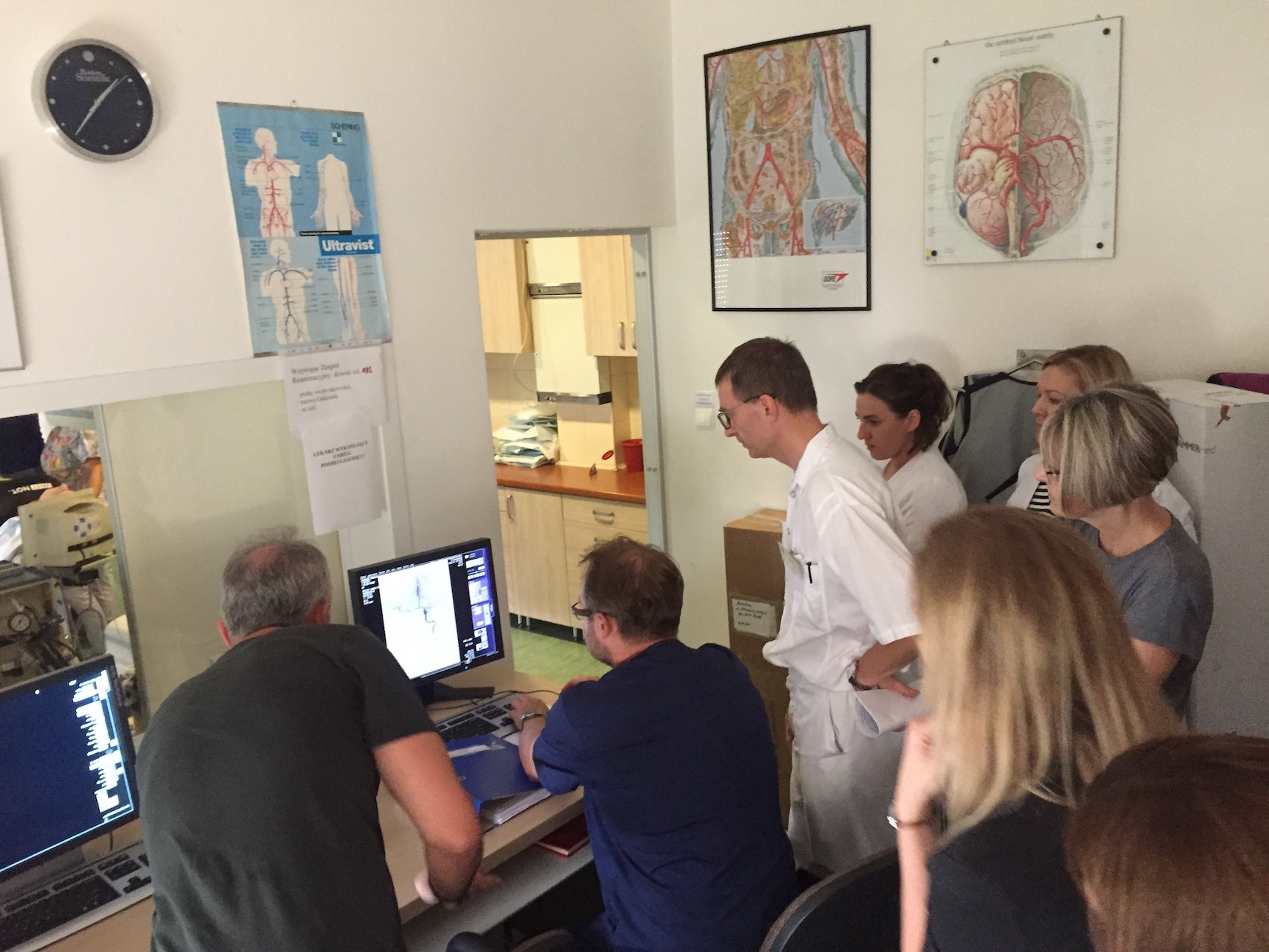
이 병원은 이미 CT에서 혈전용해술을 받은 환자를 치료하기 위해 최선을 다했으며, 이는 일반적으로 10분 정도의 DTN 시간으로 입증되었습니다. 그러나 최근에 여러 새로운 의사들이 합류했으며, 또한 새로운 뇌졸중 병동을 보유하고 처음부터 경로를 만들어야 했던 올스젠의 Clinical University Hospital 이웃에게 서비스를 제공할 기회를 보았습니다. 대학 병원은 나중에 3회 연속 다이아몬드 ESO Angels Awards를 수상했습니다.
임상 시나리오를 마무리하고 이웃을 초대하는 것 외에도, 병원 외부에서 향후 더 많은 의사를 교육하기 위해 사용할 교육용 비디오를 제작하기 위한 준비가 이루어졌습니다. 이는 다른 시뮬레이션 성과 외에도 국가 수준에서 가시성을 높일 수 있는 기회를 제공했습니다.
더 많은 노력을 기울이십시오
“환자”는 앰뷸런스 사전 알림 후 3분 시점에 병원에 도착하여 뇌졸중팀 알렸으며, 놀랍게도 도착과 첫 번째 의료 연락 사이에 지체가 없었습니다. NIHSS 스크린은 1분 후에 수행하였고, 2분 후에 코드 뇌졸중이 활성화되었다. 4분 후, 분석을 위해 혈액 검체를 실험실로 전송했다. 6분 반에 환자가 CT 스캐너로 미끄러졌습니다. 의사 결정 임상의가 결과를 분석하고 3분 30초 내에 치료 결정을 내렸습니다.
치료는 환자가 병원 문에 도착한 후 11분 시점에 시작되었으며, 혈관CT 스캔은 동시에 실시되었다. 그런 다음 시뮬레이션을 혈관실로 진행했습니다. 실제 상황에서 카테터는 40분 이내에 서혜부의 피부를 관통했습니다.
이는 인상적인 성과였으나, 항상 호전될 수 있기에, 병원에서 환자로부터 혈액 검체를 검사할 필요를 제거하기 위해 현장 INR 기기를 확보하는 데 동의했습니다.
시뮬레이션은 계획되지 않은 다른 이유로 기억에 남았습니다.
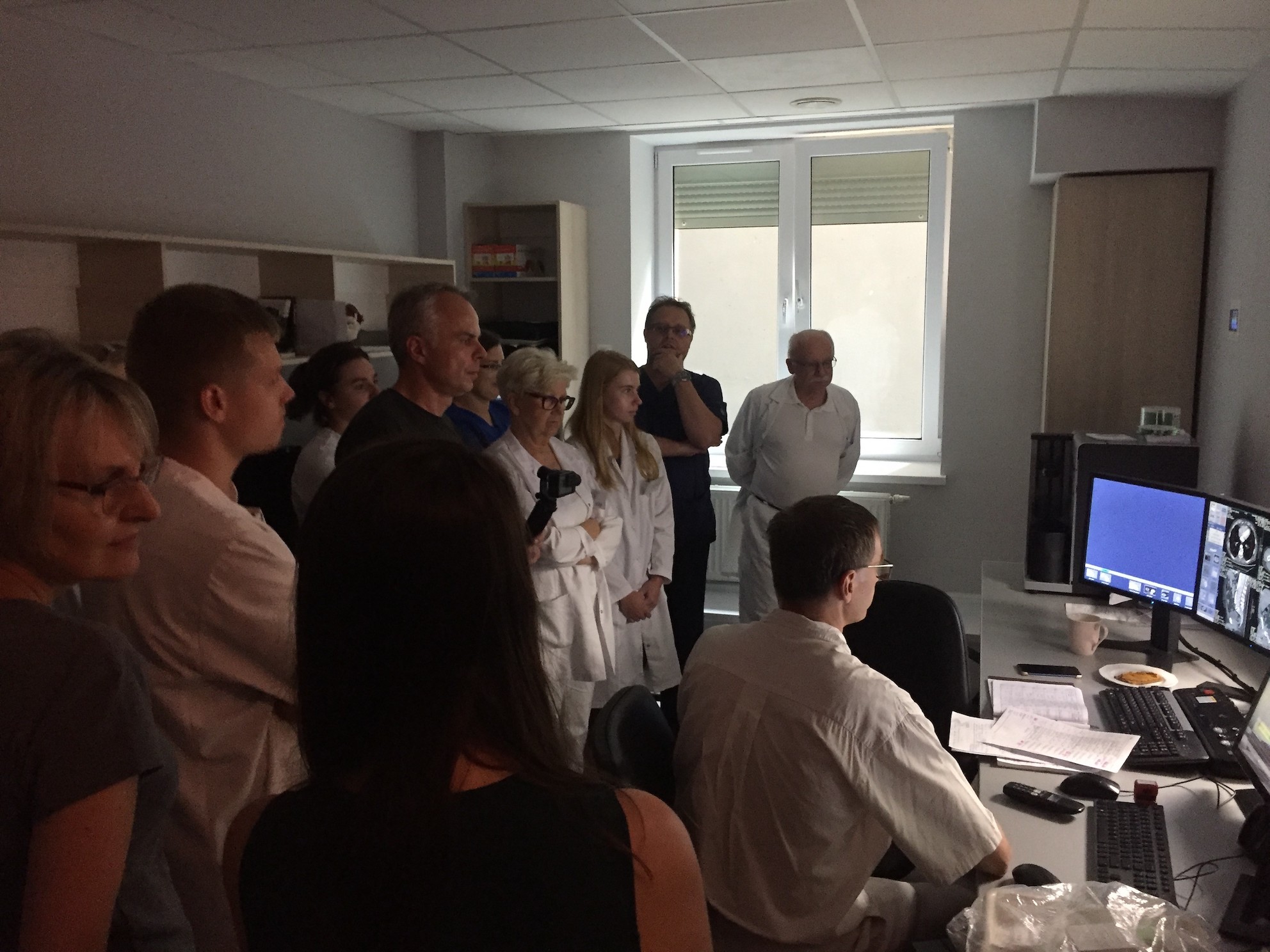
이 과정 중 두 시점에서, CT 및 angioCT 결과 해석에 있어 즉흥적인 강의를 받기 위해 20명의 이상한 의사들이 조치를 일시 중단했습니다. 게임 플랜에는 없지만, 진료실의 의사들이 의사 결정 기술을 연마하는 데 도움이 되는 일부 고급 교육에서는 어느 때보다 좋은 시기인 것 같았습니다.
삶이 위험에 처해 있을 때, 그 순간을 포착하는 것은 당연합니다.